Overview
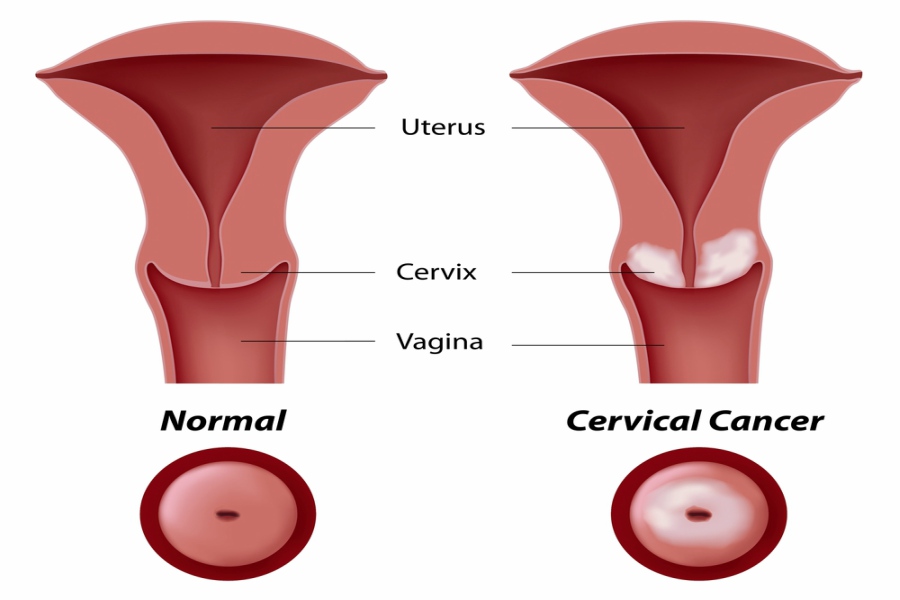
Cervical cancer is a condition that arises when the cells in the lining of the cervix (a long, narrow, cylindrical-shaped passage that connects the vagina and uterus) divide and grow abnormally. It usually affects women above 30 to 45 years.
Cervical cancer is of the following types:
- Squamous cell carcinomas: This type of cancers begins in the thin, flat cells that cover the bottom of the cervix. About 70 to 80% of cervical cancers are squamous cell carcinomas.
- Adenocarcinoma: This type of cancer develops in the column-shaped glandular cells, which lines the cervical canal. It is less common, and accounts for 20% of cervical cancer.
- Mixed carcinomas: This type of cancer have the characteristic of squamous as well as glandular cancer cells. Mixed carcinomas are rare and account for about 5 to 6% of cervical cancer.
Causes
Healthy cells grow, divide, and die at the right time and get replaced by new cells. But, when sudden changes occur in the DNA (genetic material) of cervix cells, the normal cell function gets disrupted, and the cells begin to grow and divide uncontrollably without dying, thereby resulting in the development of cervical cancer.
SYMPTOMS
No symptoms may be seen during the early stage of cervical cancer. Hence, regular pelvic examination and pap tests are advised.
- When symptomatic, the symptoms include:
- Abnormal vaginal bleeding after sexual intercourse
- Heavier menstrual periods that last longer than normal
- Vaginal discharge with the foul odor
- Pelvic pain
- Pain during intercourse
- Bleeding after menopause
DIAGNOSIS
Regular screening helps in determining any abnormal changes in the cervix, which can be treated before cancer develops. The following are theroutine tests for cervical cancer:
- Pap test: A spatula or brush is inserted inside the vagina to collect a sample of cells from the lining of the cervix. These cells are examined in the laboratory for determining any abnormalities.
- HPV DNA test: A sample of cervical cells are collected and examined to determine any infections, especially HPV. This test is an appropriate alternative to the Pap test.
If any symptoms of cervical cancer are present or the Pap test shows any abnormalities, then a colonoscopy is done.
Colonoscopy: It is an outpatient procedure, in which, a lubricated colonoscope (a thin, long, flexible tube with a video camera at one end) is inserted in the cervix to determine any abnormalities. If any abnormalities are seen, then a small sample of tissue is collected and examined.If cervical cancer is present, then the following tests are done to determine the extent of cancer:
Pelvic examination: To determine if cancer has spread to the womb, vagina, rectum, or bladder
Blood tests: To assess the kidney and liver functioning
Imaging tests: Tests, such as CT scan, X-rays, MRI to examine if cancer has spread to other organs.
Staging: The staging of cervical cancer is as follows:
- Stage 0: Cancer cells are not found in the cervix, but abnormal cell may develop into cancerous cells. This is a pre-cancerous stage.
- Stage-1: The cancer is located inside the cervix.
- Stage-2: Cancer has spread to the surrounding tissues of the cervix, but has not reached to the lining of pelvis or lower part of the vagina.
- Stage-3: Cancer has spread to the lower region of the vagina or pelvic wall.
- Stage-4: Cancer has reached into the bowel, bladder, or other organs, such as lungs.
RISK FACTORS
Human papillomavirus (HPV) infection is a common, sexually transmitted disease that increases the risk of cervical cancer.HPV produces certain proteins, which may block the action of tumour suppressor genes (genes that control the normal cell growth), thereby allowing abnormal growth and division of the cells located in the lining of the cervix.
Besides HPV, several other factors may increase the risk of cervical cancer, including:
Multiple sexual partners: Having multiple sexual partners may increase the risk of HPV infection, which is a major cause of cervical cancer.
Smoking: Chemicals released while smoking may damage the DNA of the cervix cells and increase the risk of cervical cancer.
Weakened immune system: Weakened immune system due to HIV or use of immunosuppressants increases the risk of HPV infection, which may result in cervical cancer.
Sexually transmitted disease: Diseases such as chlamydia, gonorrhea, syphilis may increase the risk of cervical cancer. Multiple pregnancies: Woman who had three or more full-term pregnancies are found to be at ahigher risk.
POST-OPERATIVE CARE
The following measures must be taken after the surgery:
- Perform breathing exercises
- Keep the wound clean and dry
- Take the prescribed medicines regularly
- Follow-up regularly
- Have a healthy diet
- Consult the doctor immediately if you notice any unusual symptoms
Common complications of surgery may include:
- Infections
- Vaginal bleeding
- Bleeding in the pelvis or abdomen
- Bowel problems
- Blood clots swelling of legs
- Numbness in the legs
TREATMENT
Based on the patient’s age, medical history, overall health, and stage of cancer, the following treatment options are available:
1. Surgery:
Early stage cervical cancers can be removed or treated with the following surgical options:
- Cryosurgery: An extremely cold cryoprobe (a long, slender surgical instrument) is inserted directly into the cervix to freeze and kill the abnormal cells.
- Conization: A heated wire loop, a scalpel, or a laser beam is used to remove abnormal cone-shaped tissue from the cervix. This surgery is recommended to treat small cervical cancers that have not spread.
- Trachelectomy: In this procedure, cervix and the upper region of the vagina are removed, whereas the uterus and ovaries are left in the place.
- Hysterectomy: It is a surgical procedure to remove all parts of the uterus. It may be of two types:
Total hysterectomy: An incision is made on the lower abdomen or on the vagina to remove the uterus and cervix.
Radical hysterectomy: An incision is made either on the abdomen or vagina to remove the uterus, cervix, and parts of the vagina. In some cases, ovaries, fallopian tubes, or surrounding lymph nodes are also removed.
- Pelvic exenteration: This surgery is done to treat advanced cancer, which has not spread beyond the pelvis.
2. Radiation therapy: High energy X-rays are used to kill cancer cells. In cervical cancer, radiation therapy can be used alone or in combination with surgery.
3. Chemotherapy: It uses medicines to kill cancer cells. Chemotherapy is usually given before the surgery to shrink the tumour or after the surgery to prevent the risk of recurrence.
FACTORS AFFECTING COST
The overall cost of cervical cancer treatment in India is 3 lakh to 10 lakh. Sometimes, when the treatment duration extends, the cost will increase.
The cost of cervical cancer surgery is 30-50% less in India when compared with other countries.


 Best Hospitals
Best Hospitals