Overview
Prostate cancer is a common cancer type of cancer in men. In this cancer, the cells in the prostate gland begin to grow uncontrollably.
Prostate is a walnut-sized gland present below the bladder in men, which produces a fluid that forms part of semen. The size of the prostate gland increases with age.
Most prostate cancers are slow-growing cancer, but in some cases, it may grow and spread fast.
Adenocarcinomas, the most common type of prostate cancer, develops from the gland cells that produce the fluid.
Some other types of prostate cancer include:
- Small cell carcinomas
- Sarcomas
- Neuroendocrine tumours
- Transitional cell carcinomas
Causes
The exact cause of the cancer is still undiscovered. It is believed that prostate cancer is caused due to a change in the DNA of the prostate gland cells.
Several factors may increase the risk of prostate cancer, such as:
- Age: The risk of prostate cancer increases with increasing age.
- Family history: A person with a family history of prostate cancer or breast cancer has an increased risk of developing prostate cancer.
- Race: Black men have an increased risk of prostate cancer than the white men do. It is also found that prostate cancer in black men is usually advanced and in a more aggressive form.
Some other possible factors that may also increase the risk of prostate cancer are:
- Obesity
- Diet rich in high-fat dairy products and red meat
- Reduced intake of fruits and vegetables
- Smoking
- Chemical exposure
- Inflammation of the prostate
- Vasectomy
- Sexually transmitted infections
SYMPTOMS
In the early stage, prostate cancer may cause no symptoms.
The symptoms of the prostate gland may vary from person to person. Some may show symptoms, and some may show no symptoms at all.
Some common symptoms of prostate cancer may include:
- Difficulty in urination
- Interrupted flow of urine
- Frequent urination (especially in night)
- Blood in the semen or urine
- Burning sensation or pain during urination
- Long-lasting pain in the pelvic region
- Erectile dysfunction
- Difficulty in emptying the bladder completely
DIAGNOSIS
A physical examination is done to detect any signs of disease or lumps. The history of any medical illness or treatment and habits is obtained. To further diagnose the condition, the following tests are performed:
- Digital rectal test: In this test, a gloved finger is inserted into the rectum to feel the prostate gland for any abnormal areas or lumps.
- Prostate-specific antigen (PSA) test: The level of PSA (a substance made by the prostate) is checked in the blood. Increased level of PSA in the blood may indicate prostate cancer.
- Transrectal ultrasound: A probe that gives off ultrasound waves is inserted into the rectum to check the prostate gland. It is usually used during the biopsy procedure (transrectal ultrasound-guided biopsy).
- Transrectal magnetic resonance imaging (MRI): A probe is inserted into the rectum near the prostate gland. The probe bounces radio waves off the tissues to create a detailed picture of the area. It is performed to evaluate if cancer has spread outside the prostate gland. It may be performed during the biopsy procedure (transrectal MRI guided biopsy).
- Transrectal biopsy: A small sample tissue is removed from the prostate gland with the help of a thin needle. After removing the tissue, it is viewed under the microscope to detect cancer cells.
After diagnosing prostate cancer, the following imaging tests may be performed to determine the extent of cancer:
- Bone scan
- CT scan
- MRI scan
- PET scan
- Ultrasound
Stages of prostate cancer
- Stage I: In this stage, cancer is in the slow growing phase. The cancer involves half or less than half of one side of the prostate gland. The PSA (Prostate-Specific Antigen) levels are low. The cancer cells look like healthy cells (cancer cells are well differentiated).
- Stage II: In this stage, cancer is more advanced than stage I, but is still present only in the prostate gland. The PSA levels are low or medium. The cancer is small in size but has an increased risk of spreading and growing. It has further three subtypes:
- IIA: In this stage, the cancer is present in one-half or less in one side of the prostate. Cancer cells are well differentiated, and the PSA levels are moderate.
- IIB: In this stage, cancer is present inside the prostate gland, and can be felt during the digital rectal exam (DRE). It has increased chances of cancer to spread and grow.
- IIC: In this stage, cancer is advanced and present only inside the prostate gland. The PSA levels are medium . The cancer cells are poorly or moderately differentiated.
- Stage III: This stage of cancer has high PSA levels. It is further divided into three sub type:
- IIIA: In this stage, cancer has spread to the nearby tissues or even seminal vesicles..
- IIIB: In this stage, cancer has spread to seminal vesicles or nearby structures (bladder, pelvic wall or rectum) or tissue from the prostate gland.
- IIC: In this stage, cancer is high grade and the cells are poorly differentiated.
- Stage IV: This stage of cancer is further divided into two subtypes:
- IVA: In this stage, the cancer spread out up to the regional lymph nodes.
- IVB: In this stage, the cancer has spread to other parts of the body like distant lymph nodes or bones.
Recurrent prostate cancer: The cancer that come back after the treatment is known as recurrent prostate cancer. It may be in the prostate gland or in other parts of the body.
In the early stage of the prostate cancer, it may show no symptoms. But, in the advanced stage, it may show symptoms like trouble in urination, blood in semen, reduced force in the stream of urine or discomfort in the pelvic region.
RISK FACTORS
The risk of prostatectomy depends on the patient’s age, body type, and health, and type of the procedure. The common risks of prostatectomy may include:
- Urinary incontinence
- Erectile dysfunction
- Decrease in penis size
- Inguinal hernia
- Impotence
POST-OPERATIVE CARE
The following measures must be taken after the surgery:
- Avoid doing physical activities for at least two months after surgery
- Perform Kegel exercise to strengthen the pelvic muscles
- Post-surgical complications:
TREATMENT
Various treatment options are available for treating prostate cancer. The choice of the treatment is based on several factors like the extent of cancer, growth of cancer, and overall health of the patient. In patients with low-risk prostate cancer, immediate treatment may not be given. Instead, they are kept on active surveillance (regular follow-up is done to monitor the progression of cancer). If in the surveillance, cancer seems to be progressing, the patient needs to undergo treatment for the condition.
The treatment options for prostate cancer are:
- Radical prostatectomy: The prostate cancer, along with some surrounding tissue and lymph nodes, are removed. The prostatectomy can be performed in the following ways:
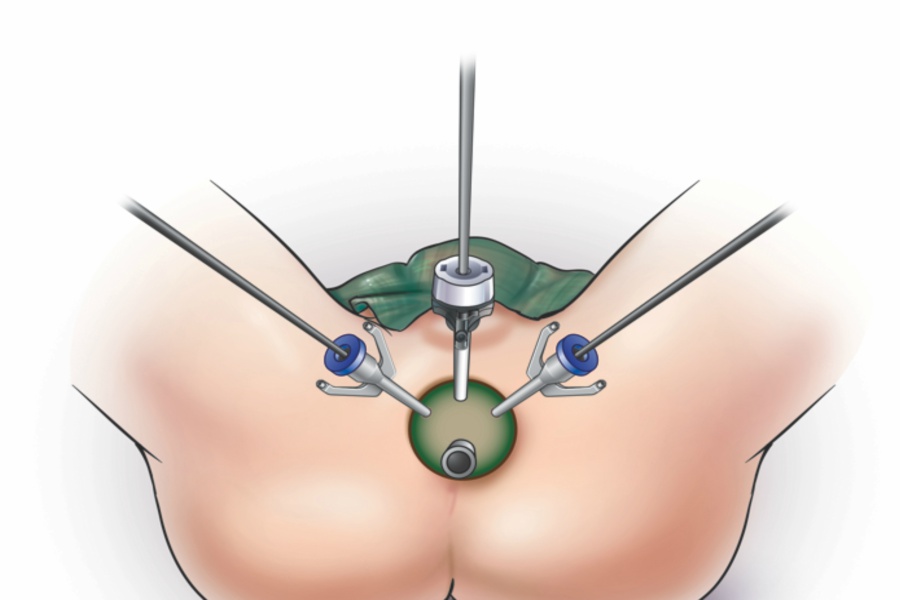
- Robot-assisted surgery: In this method, the instruments are attached to a robot (mechanical device), which are inserted into the abdomen through numerous small incisions. The doctor guides the robot to move the instrument. It aids in making more accurate movements.
- Retropubic surgery: In this method, an incision is made at the lower abdomen through which the prostate gland is taken out.
- Perineal prostatectomy: An incision is formed in the perineal wall (the area between the scrotum and anus) to remove the prostate gland.
Radiation therapy:
High-energy X-rays or proton beams are used to kill the cancer cells or hinder their growth. It can be given in two ways:
External beam radiation: A machine is used to deliver radiations to the cancer area externally.
Brachytherapy: A radioactive substance that is sealed in seeds, wires, needles, or catheter is placed in the prostate tissue by using a needle guided by ultrasound images. These seeds deliver low-dose radiation for a long duration.
Hormone therapy
The hormones are removed or blocked from performing their actions, which stops the cancer growth. In prostate cancer, surgery, drugs or other hormones are used to remove or block the action of the male sex hormone, testosterone (responsible for the growth of prostate cancer). It is usually given in case of advanced cancer to reduce the size or slow down the growth of cancer.
Hormone therapy may be given in the following ways:
- Luteinizing hormone-releasing hormone (LH-RH): These medications prevent the production of testosterone. The drugs used in the hormone may include goserelin, leuprolide, triptorelin and histrelin. Sometimes, some other drugs like ketoconazole and abiraterone may also be used.
- Anti-androgens: The anti-androgens like bicalutamide, nilutamide, and flutamide prevents testosterone from reaching the cancer cells.
- Orchiectomy: The testicles (part of the male reproductive system that makes testosterone) are removed. It reduces the testosterone levels in the body.
Chemotherapy:
Drugs are used to kill cancer cells. It can be administered intravenously or orally. It is beneficial in cases where cancer has spread to other body parts or when cancer does not respond to hormone therapy.
Immunotherapy (Biological therapy):
The body’s immune system is enhanced to fight against the cancer cells. Sipuleucel-T is a type of immunotherapy used to treat recurrent or metastasize prostate cancer.
Duration of the treatment
The duration of the treatment may vary for every surgical procedure. If required, radiation therapy may be given for 5 days in a week for several weeks. Chemotherapy cycles may be given based on the severity of cancer. Each cycle(which includes the treatment period and the rest period) may last for a few weeks.
FACTORS AFFECTING COST
The cost depends upon:
- The types of treatment
- The type and extent of surgery
- The types of anaesthesia
- The technology used
- The need for chemotherapy and radiotherapy


 Best Hospitals
Best Hospitals